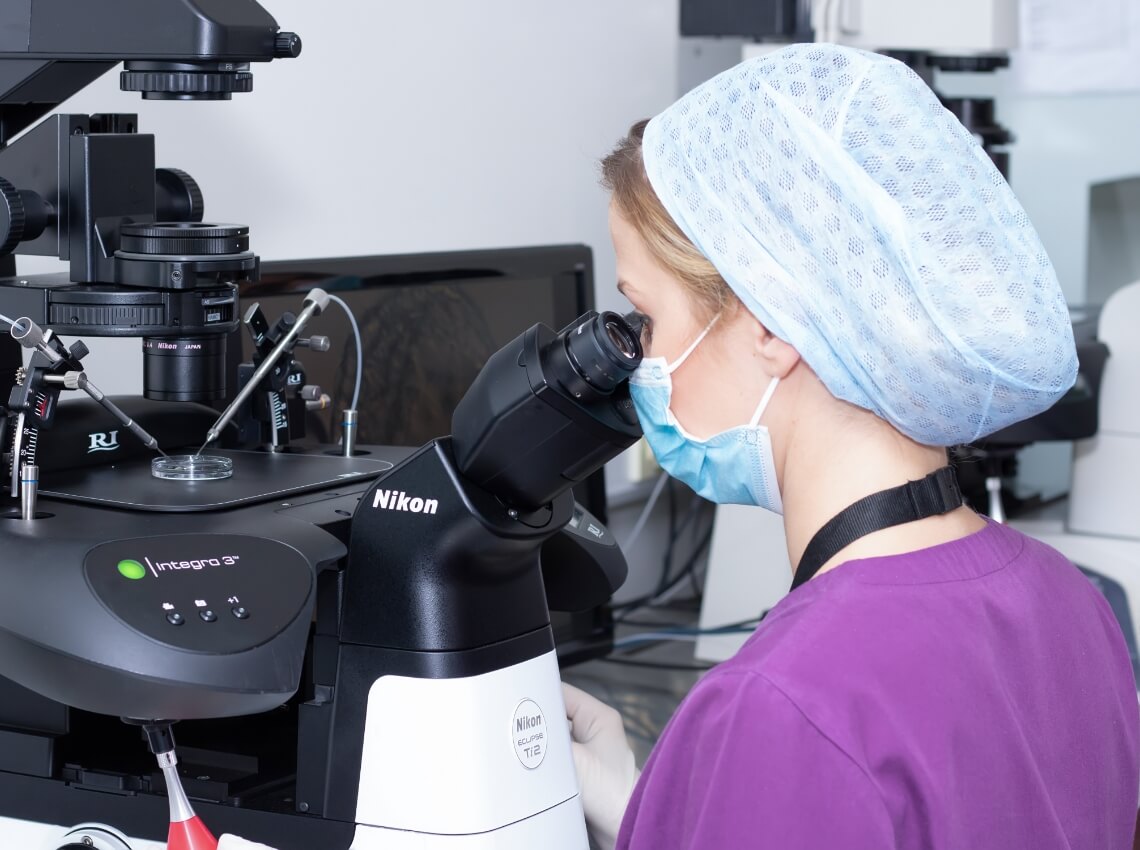
IVF can be used to overcome a wide range of challenges that may otherwise make it difficult to conceive naturally. By combining the eggs and sperm in our laboratory we can create the optimal environment for fertilisation to occur.

Fertility & IVF Treatments

In Vitro Fertilisation
(IVF)
IVF can be used to overcome a wide range of challenges that may otherwise make it difficult to conceive naturally. By combining the eggs and sperm in our laboratory we can create the optimal environment for fertilisation to occur.
Check out the 5 steps of IVF below:
Ovarian preparation
Egg collection
Embryo development
Embryo transfer
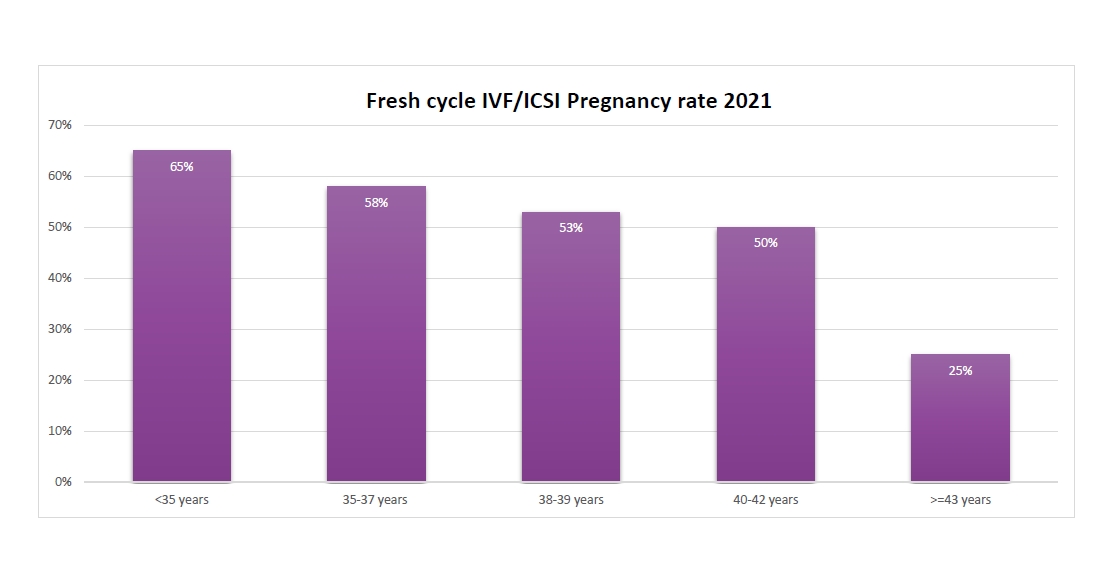
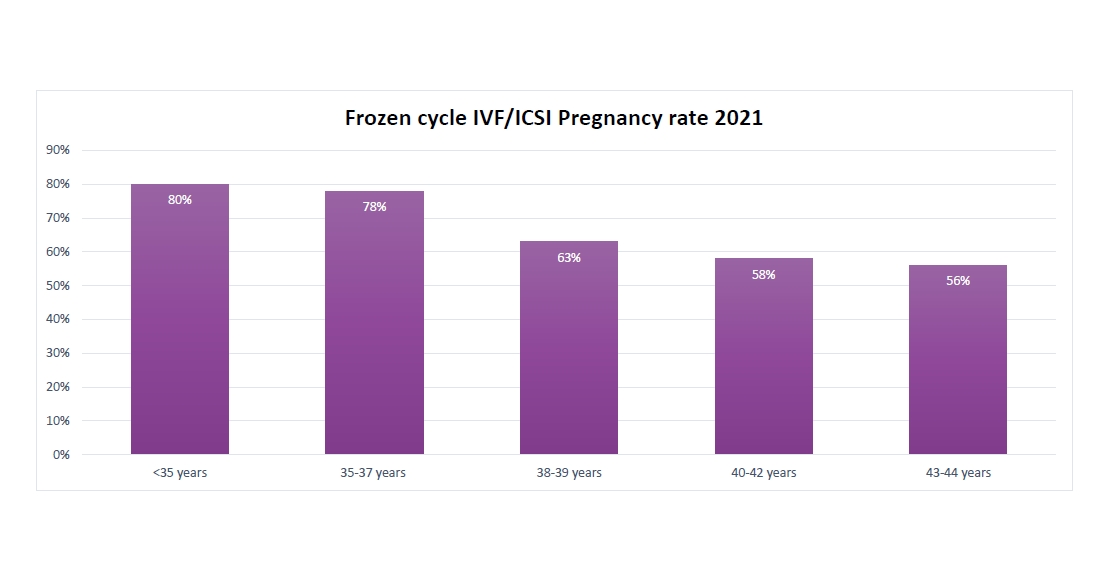
There are two ways to transfer the embryo: fresh or frozen embryo transfer. Either the embryo can be transferred back to the uterus five days after the egg collection procedure, or the embryo(s) can be frozen and thawed for transfer at a later date.
Pregnancy test
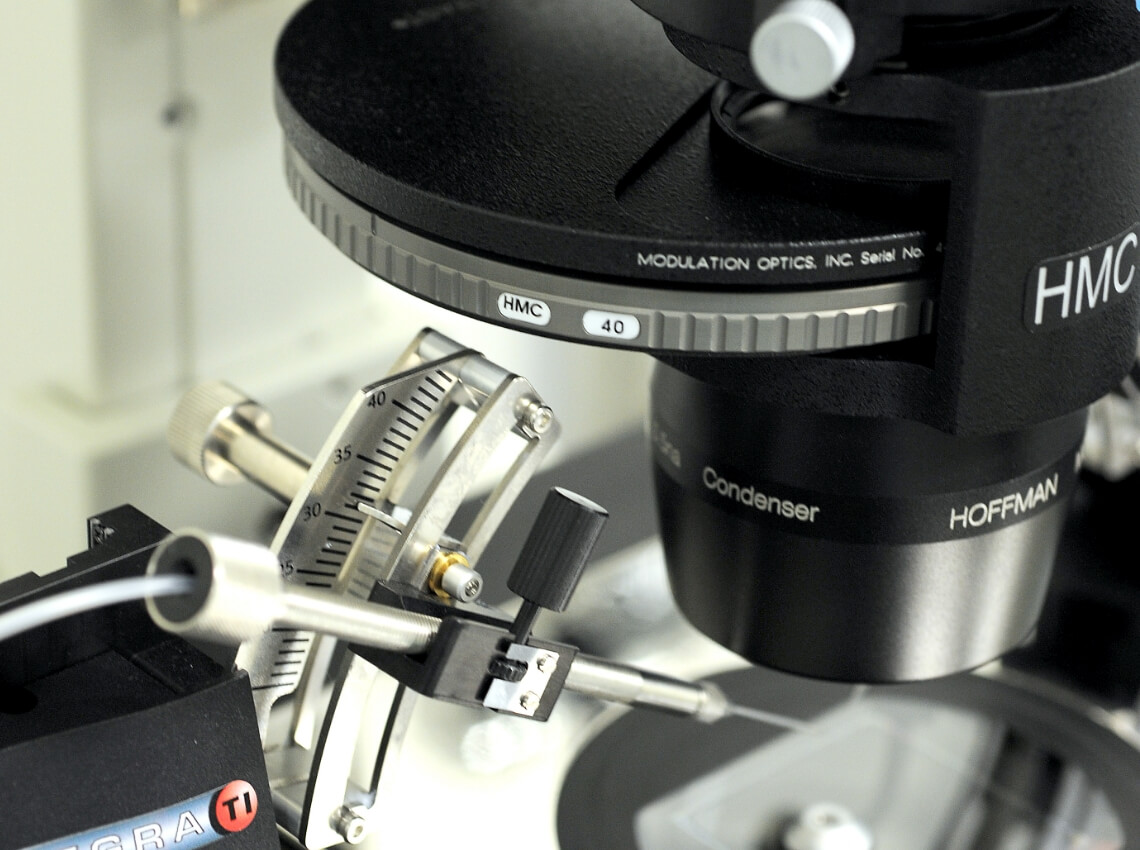
Intra Cytoplasmic Sperm Injection (ICSI)
ICSI is a technique which involves selecting a single sperm and injecting it into the egg. It is recommended in cases of severe male infertility and where there have been cases of no fertilisation following IVF previously. The fertilised embryos are allowed to develop as in standard IVF prior to transfer, freezing or further genetic testing.

Natural IVF
Natural cycle IVF is a treatment cycle where the aim is to collect the single egg produced monthly in a patient with regular cycles, without the stimulating drugs. The risk of natural IVF is the high cancellation rate due to no embryo being available for transfer from a single egg or premature ovulation.

IVF with Egg Donors
There are many reasons why someone might need to use donated eggs in their IVF journey. For example, women with low ovarian reserve, poor egg quality or medical treatment earlier in life which impacted their fertility. These women might select to use donor eggs to improve their chances of becoming pregnant.
Check out the stages of egg donation treatment below.
Consultation and donor search
Our coordinators will work with you to assist in finding the right donor for you. Your chosen donor will then undergo tests, stimulation and egg collection, resulting in eggs ready for use in your IVF cycle.
Our egg donation program also has a database with frozen eggs available for immediate use.
Recipient screening
Fertilisation and embryo development
Embryos typically develop for 5 or 6 days prior to transfer or freezing. Our embryologists are in constant contact with you during this time to update you on your embryo's development.
Embryo transfer
There are two ways to transfer an embryo: fresh or frozen embryo transfer. Either the embryo can be transferred back to the uterus five days after the fertilization, or the embryo(s) can be frozen and thawed for a transfer at a later stage. The embryologist will help you to decide which embryo is the best to transfer for the highest possible chance of a healthy and successful pregnancy.
Pregnancy test
IVF with Sperm Donor
Our sperm donation team will work with you to explain your options and assist in finding the right donor. Partnering with accredited international sperm banks, we ensure high-quality sperm selection from donors of all races and ethnicities.
Using donated sperm in the IVF process gives more people the opportunity to start a family. Reasons for needing donated sperm include genetic disorders or being single woman. Our expert team will guide patients through every step, from finding the right donor to undergoing IVF.
Check out the stages of sperm donation treatment below.
Consultation and sperm donor search
Recipient screening and Ovarian preparation
Egg collection
Fertilization and embryo development
Embryo transfer
Pregnancy test

Intrauterine insemination (IUI)
Intrauterine Insemination (IUI) treatment can help patients to start their family using either a partner or donor’s sperm. It’s a quick treatment and should cause no more discomfort than a pap test.
Prior to carrying out IUI your doctor will recommend some medical investigations to confirm that this treatment type is suitable for you.

Fertility Preservation
Preserving your fertility involves freezing your eggs, sperm or embryos so that you can hopefully have a biological family in the future.
Egg freezing
Egg freezing is an opportunity for every woman to preserve the ability to have children later in life. Reasons to freeze your eggs:
- Women who need treatment for cancer or another treatment that may affect their ability to get pregnant
- Women faced with premature menopause
- Women who may wish to postpone childbearing
- Those undergoing IVF with religious or ethical concerns over embryo freezing
Check out the stages of egg freezing below
Consultation
Blood tests, sperm analysis and investigations
Ovarian preparation
Egg collection
Egg freezing and storage
PGT Testing
Pre-implantation genetic testing (PGT) is a comprehensive test offered to couples undergoing IVF for the simultaneous detection of monogenic diseases (PGT-M), numerical abnormalities (PGT-A) and structural rearrangements (PGT-SR) in fertilised embryos at the blastocyst stage (day 5/6 stage).
Check out below.
PGT for monogenic disorders
Who should undergo PGT-M
Only couples with a known genetic mutation in the family that can be inherited to their offspring should perform this testing. Examples of inherited genetic diseases that can be identified with PGT-M are Thalassemia, Cystic fibrosis and Tay-Sachs disease.
PGT for aneuploidy
Who should undergo PGT-A
- Women of advanced age as they have higher chances of chromosomal aneuploidies due to the aging of their eggs
- Couples with recurrent miscarriages
- Couples with multiple IVF failures
- Men with severe oligozoospermia (low sperm count)
PGT for chromosomal structural rearrangements
Who should undergo PGT-SR
Couples who are carriers of a balanced translocation or inversion (either one or both partners).