1
Consultation
An initial consultation is the first step. In this appointment you will find out about the sperm donation procedure - options, selection process and costs.
2
Finding your donor
Our sperm donation team will work with you to explain your options and assist in finding the right donor for you. We work with accredited international sperm banks, and we ensure the selection of high-quality sperm from sperm donors of all races and ethnicities.
3
Blood tests and investigations
Your doctor will recommend some tests and investigations to ensure you are ready for treatment. These typically include a hormonal profile test, ovarian reserve test and an ultrasound scan.
4
Ovarian preparation
Most patients will undergo a course of medication and monitoring which will help ensure the best possible results. During this period, you will have scans and blood tests to ensure the best outcome.
5
Egg collection
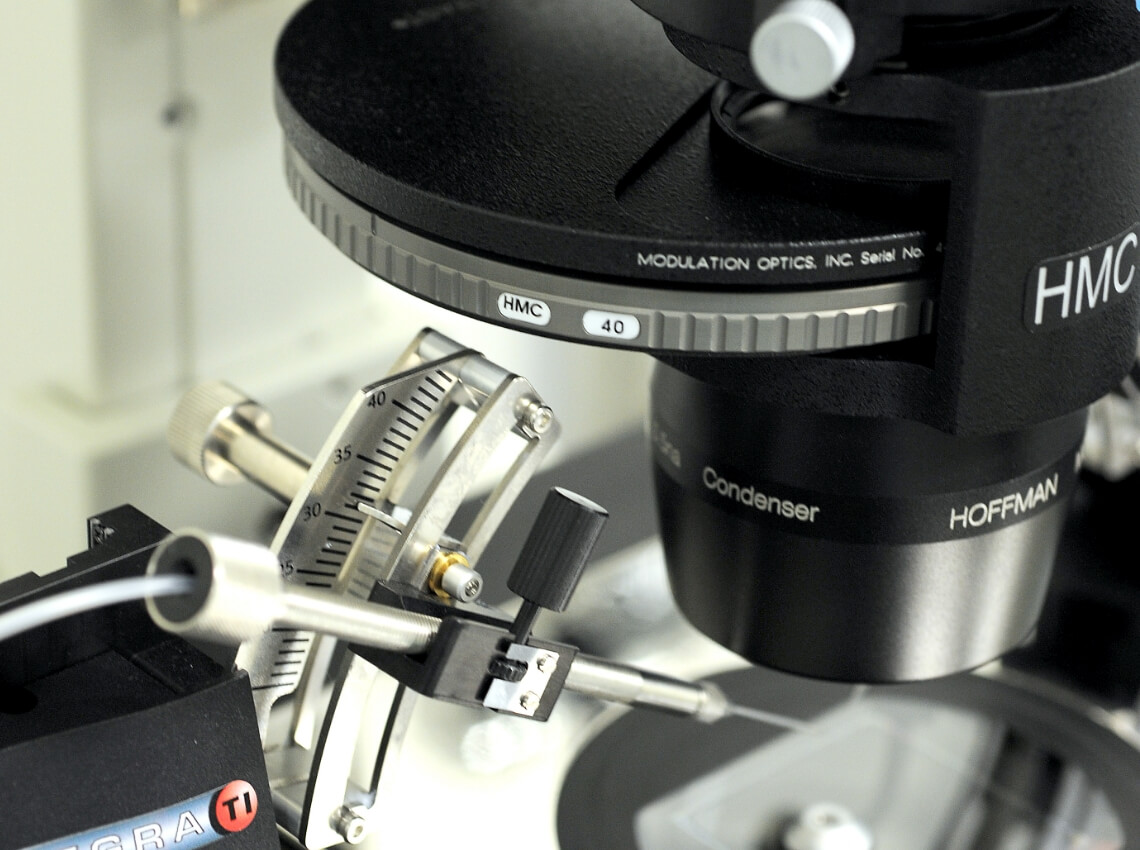
Having monitored your blood and scan result, your doctor will decide when the optimal time is to collect your eggs. The procedure involves collecting eggs from the woman’s ovaries using a needle that is passed through the vagina and into each ovary under ultrasound guidance and deep sedation. On the day of the egg collection, the eggs will be fertilised with donor sperm in the laboratory.
6
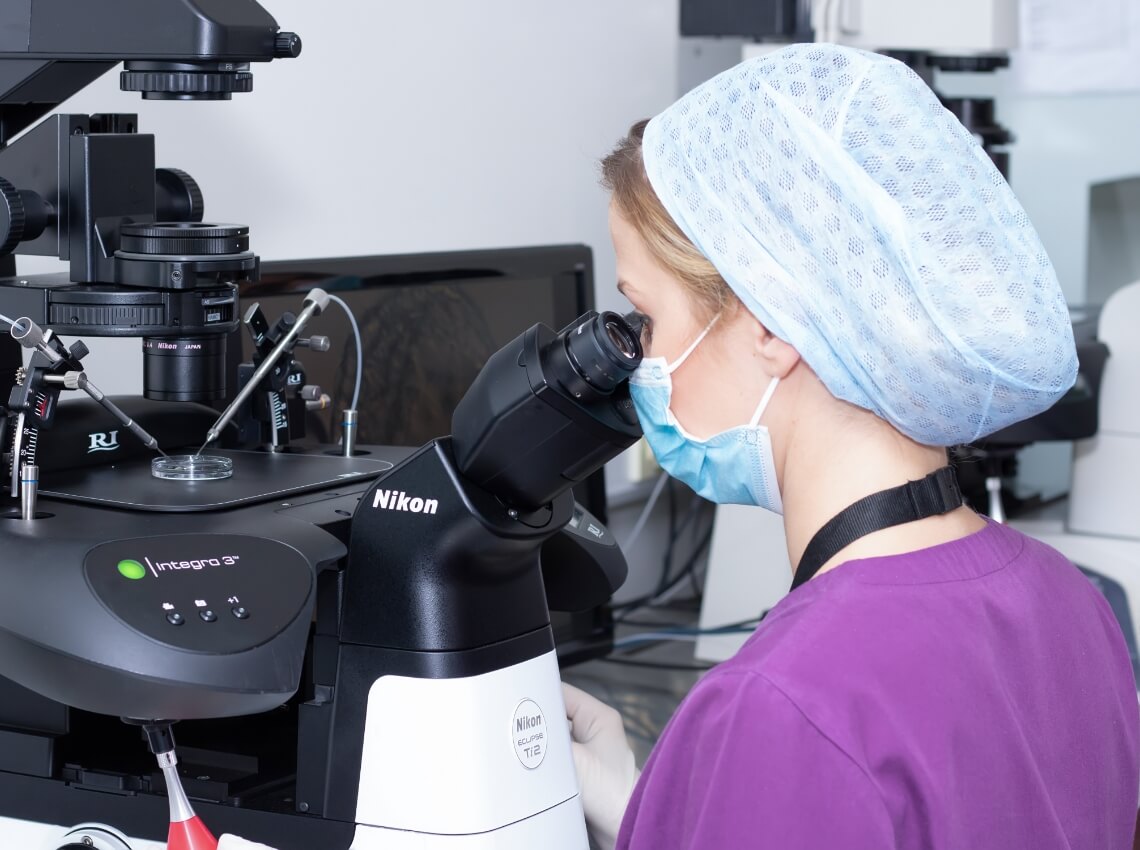
Embryo development
Once fertilised, embryos typically develop for 5 to 6 days prior to transfer or freezing. Our highly experienced embryologists are in constant contact with you during this time to update you on your embryo's development.
7
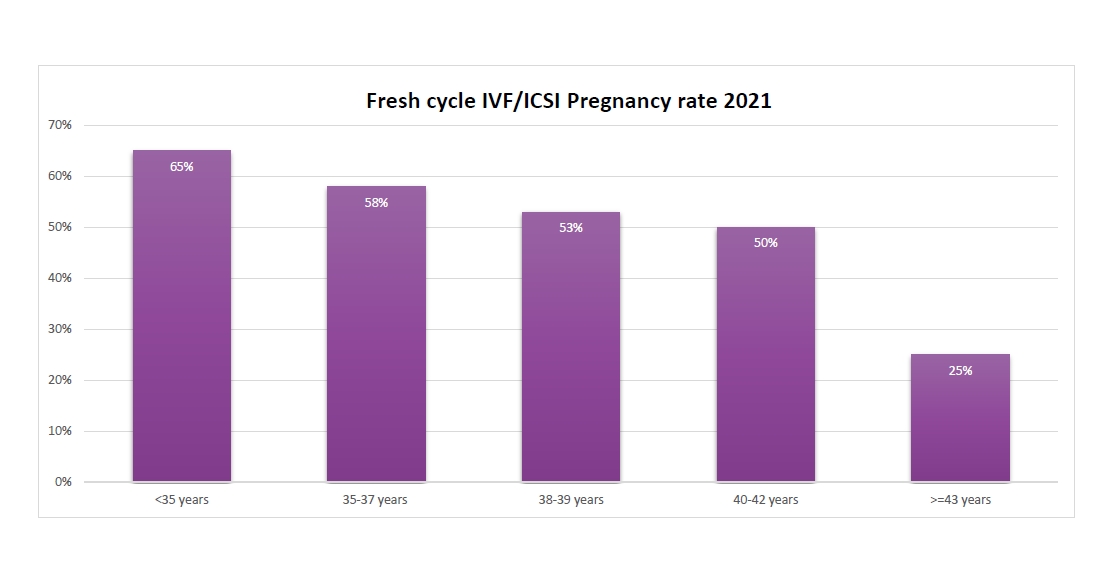
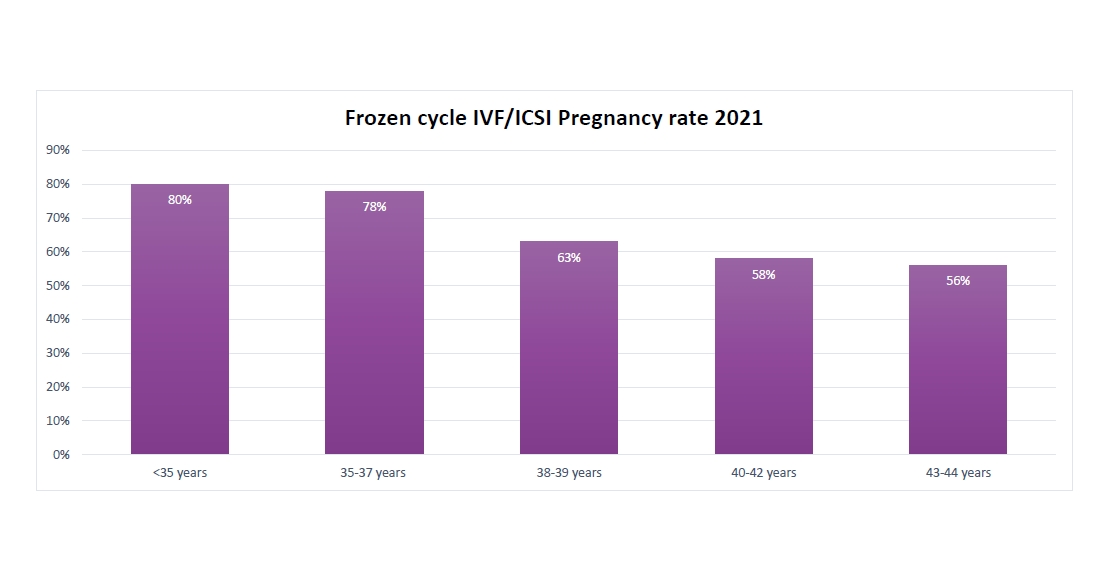
Embryo transfer
One or two embryos can be transferred with a thin catheter back to the uterus. The procedure is simple and takes less than 10 minutes. There are two ways to transfer an embryo: fresh or frozen embryo transfer. Either the embryo can be transferred back to the uterus five days after the egg collection procedure, or the embryo(s) can be frozen and thawed for a transfer at a later date.
8
Pregnancy test
9 days after your embryo transfer you will take a pregnancy test which will confirm the results of your treatment. Whatever the outcome, our team of doctors, embryologists, nurses and counsellors will be on hand to support you in your next steps.